 Aromatase inhibitors (AIs) are an important component of the treatment of hormone receptor-positive breast cancer in females.
Aromatase inhibitors (AIs) are an important component of the treatment of hormone receptor-positive breast cancer in females.
At the same time, they are necessary to prevent aromatization (estrogenic activity) caused by androgenic anabolic steroids (AAS).
The first class of anti-estrogenic drugs are Selective Estrogen Receptors Modulators (SERM’s), which act selectively in certain tissues (tamoxifen, clomiphene), occupying the estrogenic receptors, thus making circulating estrogens unable to attach to the receptors.
Modern aromatase inhibitors include irreversible steroidal inhibitors (exemestane) and non-steroidal inhibitors (anastrozole, letrozole), which inhibit the action of aromatase enzyme that converts androgens to estrogens.
Aromatisaton takes place in a variety of tissues, such as mammary gland, adipose tissue, liver and brain.
These drugs have the ability to diminish peripheral-circulating estrogens and beta estradiol (E2) in particular.
E2 is the main representative of estrogens.
During a precontest preparation, or “cutting phase” AIs are widely abused.
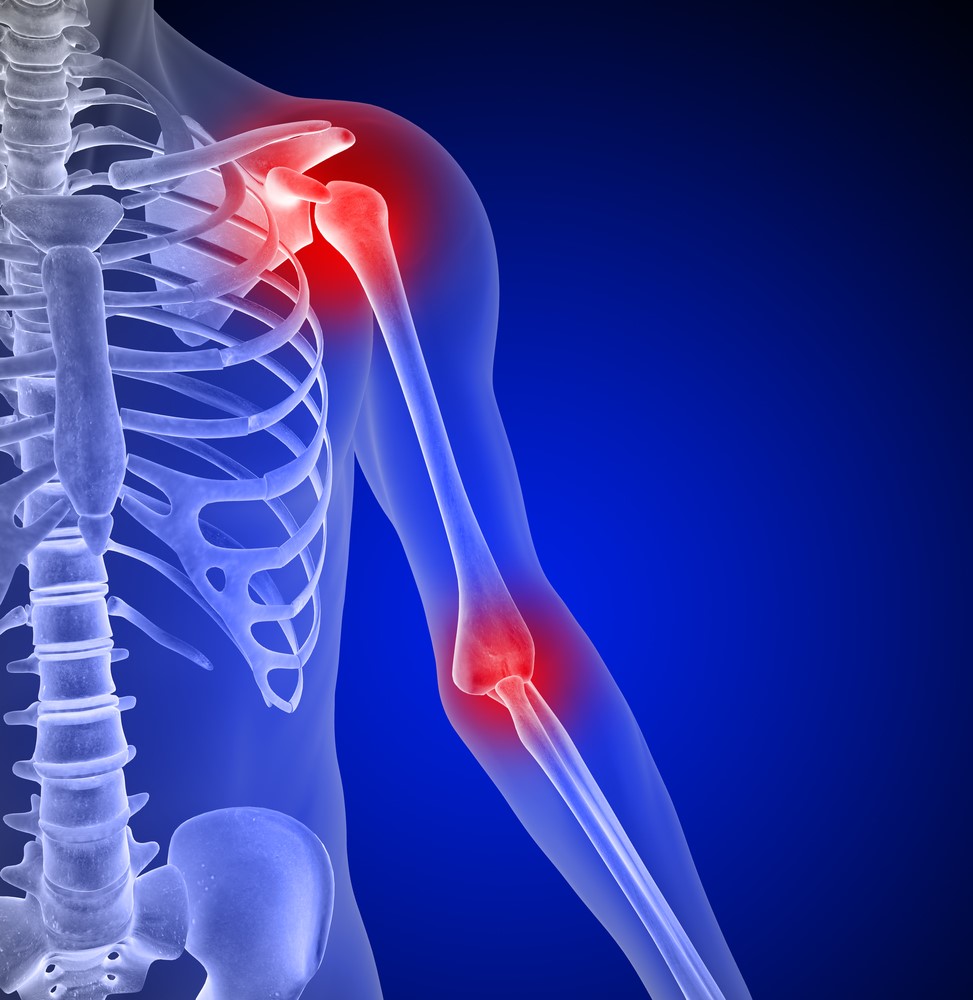
This leads to a plethora of different side effects, with “arthralgia of aromatase inhibitors” being a common toxicity.
The symptoms include joint pain, with most frequent in the wrists, knees, ankles, elbows and shoulders.
This discomfort is usually symmetrical.
Other symptoms include morning stiffness, muscle pain, skull and neck aching, carpal tunnel syndrome and restricted mobility of the affected part.
The average time of the appearance of symptoms is about 4 weeks.
Studies showed significantly higher rates of carpal tunnel syndrome following the use of anastrozole and exemestane compared to tamoxifen.
Laboratory tests and imaging examinations are normal and necessary to exclude conditions that require immediate attention, such as traumatic, inflammatory, autoimmune arthritis, fracture, mechanical derangement, or tumor.
The pathogenic mechanism of AIs -induced arthralgia has different origins:
- Firstly, we know that estrogens and aromatisation particularly, are associated with water retention and edema.
This is a beneficial environment for the synovial cavity, since joints are lubricated, and thus friction is diminished.
- Moreover, studies have shown that estrogens are natural pain inhibitory receptors, an evolutionary adaptation to help women to better tolerate the pain during childbirth, when estrogen levels are particularly high.
Thus estrogen deprivation makes the body more vulnerable to pain sensation and decreases threshold for painful stimuli.
The perception of pain is more intense.
Scientific evidence shows that, AIs do not cause actual harm to the joint destruction of articular surfaces, cartilage, ligaments and muscles surrounding.
Therefore, discontinuation of the AIs leads to prompt relief of symptoms.
The most appropriate intervention for pain management in AIs-associated arthralgia may be a combination of pharmacologic approaches in conjunction with dietary supplements for bone protection.
- As an alternative treatment the use of SERMs is proposed, since these drugs act selective estrogenic on the liver and anti-estrogenic on the breast tissue.
Tamoxifen occupies the estradiol receptor, without blocking the action of aromatase enzyme in the breast and subcutaneous tissues.
Estrogens still can circulate in blood; therefore joints do not become dry.
- The use of hyaluronic acid in liquid form acts as a moisturizer, when combined with hydrolyzed collagen.
Also glucosamine-chondroitin-MSM complex helps.
These are glycoproteins, which moisturize the articular surfaces and the hyaline cartilage.
The use of ascorbic acid in ester form of vitamin C contributes to the biosynthesis of collagen protein.
- Non-steroidal anti-inflammatory drugs (NSAIDs), on the one hand suppress the inflammation and pain, since they inhibit inflammatory cytokines (prostaglandins).
On the contrary, they sabotage the phenomenon of muscle inflammation and also account for increased risk of upper gastrointestinal bleeding (stomach, duodenum).
As an alternative, omega 3 PUFAs (DHA/EPA) coming from fish oil may be used.