 As we age, our hormonal profile corresponds to the process of ageing.
As we age, our hormonal profile corresponds to the process of ageing.
In both sexes, steroid hormones, androgens and estrogens are reduced and the typical midlife crisis exists, menopause and andropause.
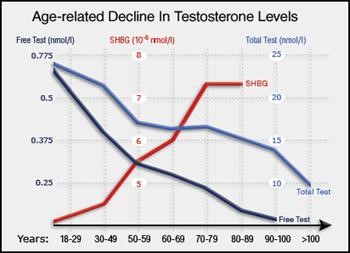
After the age of 35, the average age-related reduction in total testosterone is 10% per decade.
The symptoms that characterize andropause syndrome are:
depression-melancholy, decline in cognitive function (foggy mind), decreased libido and energy, erectile dysfunction, decreased Bone Mineral Density (BMD) -osteopenia, reduced muscle mass and strength-sarcopenia, fatigue, weakness, gynecomastia and increased visceral-omental abdominal fat.
The majority (98%) of testosterone is bound to Sex Hormone Binding Globulin (SHBG), a protein which transports it into the blood serum.
A very small percentage (2%) remains free and unbound form.
The higher rate of free-bioavailable testosterone (FT) is free, the better the libido and muscle strength will be.
Only free testosterone binds to the androgen receptor (AR) in the cytoplasm.
Therefore, free testosterone and SHBG values are inversely proportional.
As we age, serum levels of SHBG increase and free testosterone decrease, which represent one of the laboratory findings of andropause.
This is justified by the sarcopenia-cachexia-muscle wasting and concurrently the increase of the subcutaneous, adipose tissue, which elevates serum levels of beta estradiol (E2).
Therefore, the elevation of beta-estradiol (E2) increases SHBG and reduces the FT.
Hormone replacement therapy (HRT) is one of the parameters of proper age management, thus contributing to the hormonal balance of the middle-aged crisis.
Each subject with hypogonadism should be individually studied and counseled after the evaluation of certain hormonal serum levels.\
Each case is unique and one size does not fit all.
Hormonal assessment includes levels of Lutelizing Hormone (LH), Follicle Stimulating Hormone (FSH), Total Testosterone (TT), Free Testosterone (FT), Sulfate Dihydroepiandrosterone (S-DHEA), Sex Hormone Binding Globulin (SHBG), Estradiol (E2) and Prolactine (PRL).
Primary hypogonadism is characterised by normal or elevated levels of LH, FSH, while total and free testosterone levels are low.
This practically is translated into smaller testicles with normal spermatogenesis.
In primary hypogonadism, we usually administrate HCG, followed by clomiphene citrate for a couple of weeks, in order to restore hypothalamic-pituitary-gonadal axis (HPTA).
Secondary hypogonadism is characterised by low levels of total and free testosterone associated with low levels of FSH and LH, since the patient’s HPTA is shut off.
S-DHEA is usually low.
‘’Late onset’’ hypogonadism (LOH) is a mixed (primary/secondary) form of hypogonadism,
where a central (deficient GnRH and gonadotropin activity) and a peripheral (impaired steroidogenesis) component are often simultaneously present.
Regarding androgenic-anabolic steroid (AAS) abusers, they initially develop primary hypogonadism, which gradually turns into secondary or late onset hypogonadism.
This condition is also defined as ‘’androgen induced hypogonadism”, since it develops as a result of chronic abuse of AAS.