 Homocysteine (Hcy) is a sulfur amino acid, which is biosynthesized during the metabolism of methionine to cysteine mainly involving the B complex vitamins.
Homocysteine (Hcy) is a sulfur amino acid, which is biosynthesized during the metabolism of methionine to cysteine mainly involving the B complex vitamins.
It is a toxic residue of the metabolism, linked to cardiovascular disease, when accumulated.
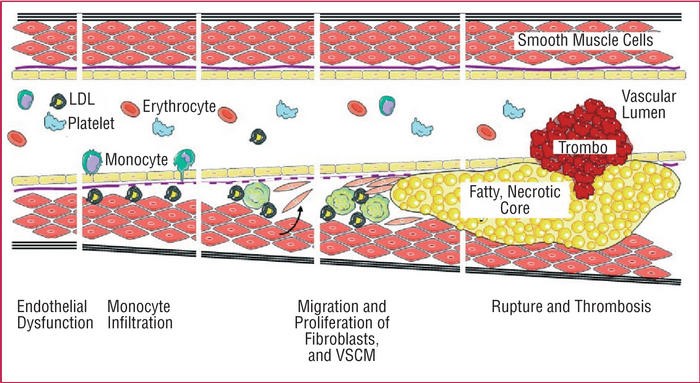
Hyperhomocysteinemia induces endothelial injury and endothelial dysfunction, increased platelet activation at the site of microvascular injury, leading to the development of atherosclerosis.
Elevation of plasma Hcy levels creates a condition called hyperhomocysteinemia (HHcy), which is characterized into three ranges; moderate (16-30 μmol/L), intermediate (31 – 100 μmol/L) and severe (>100 μmol/L) HHcy.
Hyperhomocysteinemia in combination with other factors (hyperlipidemia, hypertension, smoking, unhealthy diet, stress) promote atherogenesis, atheromatosis and atherosclerosis, that eventually lead to coronary artery disease, peripheral artery disease, stroke, or venous thrombosis.
Recent studies have shown that, a 25% elevation (about 3 μmol/L) of homocysteine’s levels is associated with a 10% higher risk of cardiovascular events and a 20% higher risk of stroke.
When these concentrations exceed 15 μm/l, there is a 25% increase in mortality.
Furthermore, homocysteine is a significant, independent risk factor for Alzheimer’s disease, Parkinson’s disease and metabolic syndrome.
Anabolic‐androgenic steroid (AAS) use has long term effects on plasma concentrations of homocysteine.
Elevation of homocysteine levels depends on:
a) the type of the AAS:
The 17 alkylated AAS are hepatotoxic and disrupt the metabolism of Hcy in the liver.
Those that aromatize (methyldrostenolone, oxymetholone?) increase estrogen (E2) concentration and reduce levels of cobalamine (vitamin B12) and folate.
Deficiencies in plasma folate and B12 have been shown to lead to elevated Hcy concentrations.
b) the duration of use:
There is a significant linear relationship between long term AAS abuse and hyperhomocysteinemia.
Administration > 6 months leads to an increase of plasma levels of Hcy.
c) the dosage of AAS
Studies have shown acute hyperhomocysteinaemia in bodybuilders using supraphysiological doses of various AAS preparations.
d) the simultaneous use-stacking of several different AAS
The mechanism of hyperhomocysteinemia during or after AAS abuse is multifactorial.
AAS are known to cause marked dyslipidemia, with significant reduction in high density lipoprotein (HDL) and an increase of low density lipoprotein (LDL) increasing the susceptibility to cardiovascular events.
Moreover, AAS affect the haemostatic system, through an increased fibrinolytic activity and simultaneously platelet aggregation.
The activation of the coagulation cascade leads to prolonged bleeding time (INR, PT are remarkably elevated).
AAS influence the hematological system leading to erythocytosis, by stimulating bone marrow and by promoting erythropoietin synthesis in the kidney.
Erythocytosis is associated with blood viscosity, thus coronary, peripheral artery and venous thrombosis.
Synthesis of homocysteine occurs in erythrocytes, thus their higher number contributes to homocysteinemia.
To address hyperhomocysteinemia, the AAS user should use vitamin B12, folate and betaine (trimethylglycine) supplementation.
Moreover, he should avoid alcohol consumption and all other factors that damage the vascular endothelium such as smoking, hypertension, dyslipidemia.
It should be noted that, although the the AAS cessation leads to reduced homocysteine levels, the damage of the vascular endothelium is irreversible.